Gut health has recently been identified as a significant determinant of overall wellness, influencing various aspects of physical and mental health. Most people believe that bacteria are the cause of illness or disease. However, beneficial bacteria in the intestines that carry out the digestive process help many vital organs. They aid digestion, improve gut immunity, reduce inflammation, and more.
Having a healthy gut plays an important role in maintaining a healthy lifestyle, including good health and a happy mind. Your gut’s impact on health is significant because the gut-brain axis connects your body and mind.
Making some simple lifestyle changes can improve gut health and maintain a balanced microbiome, thus reducing the risk of mood swings, fatigue, stomach problems, digestion, and shortness of breath during exercise.
When it comes to women’s wellness, the link between gut health and overall well-being becomes even more crucial. In this article, we examine the connection between gut health and women’s health, exploring how gut health can positively impact overall women’s health.
Understanding Women’s Wellness
Women’s wellness encompasses a range of factors, including reproductive health, hormonal balance, mental well-being, and longevity. Unlike men, women undergo unique physiological changes throughout their lives, from puberty to menopause and beyond. These changes necessitate a deeper understanding of women’s health needs and the factors that influence them.
How does gut health affect women’s wellness?
Gut health significantly influences women’s wellness in various ways:
- Nutrient Absorption: A healthy gut aids in absorbing essential nutrients, contributing to overall well-being.
- Immune Function: The gut plays a crucial role in supporting the immune system, impacting women’s ability to fight off infections and diseases.
- Mood Regulation: The gut-brain connection affects mood regulation, with a healthy gut linked to better mental well-being in women.
- Inflammation Control: Maintaining gut health helps regulate inflammation levels, reducing the risk of chronic diseases common in women.
- Hormonal Balance: Gut health influences hormone levels, impacting menstrual health and reproductive function in women.
- Dietary Choices: Women’s dietary choices influence gut health, emphasizing the importance of a balanced diet rich in fiber and probiotics.
- Personalized Wellness: Tailoring gut health strategies to individual needs can optimize women’s overall wellness.
Does Gut Health Affect the Brain?

Yes, gut health does affect the brain. This is proved by research highlighting the intricate communication between the gut and the brain, known as the gut-brain axis. The gut is home to a complex ecosystem of microorganisms that play a crucial role in various bodily functions, including digestion, immune response, and even mood regulation.
What is the gut-brain connection?
The gut-brain axis is a network that connects the digestive system with the brain, allowing for the exchange of information through the nervous system, hormones, and the body’s immune responses. Recent research has shown that the gut microbiome, which consists of various microorganisms in the gut, plays a crucial role in this communication process. Imbalances in the gut microbiome have been linked to various psychological issues such as anxiety, depression, and mood swings, particularly among women.
Gut microbes produce or help produce many of the chemical neurotransmitters that convey messages between your gut and brain. They also produce other chemicals that can affect your brain through your bloodstream. Your brain and gut, in turn, can affect your gut microbiome by altering its environment.
Does gut health affect mental health?
Yes, the gut microbiome directly affects a person’s mental health.
The balance of gut bacteria plays a significant role in a person’s mental well-being, affecting mood, thoughts, emotions, and behavior. This balance can help reduce the impact of mental health issues like anxiety, depression, and ADHD. Many researchers have studied the connection between gut health and mental well-being, particularly how it influences mood disorders and cognitive development.
Changes in the gut microbiome, especially certain bacterial strains in the digestive system, have been linked to anxiety and depression. Research shows that adopting a healthy diet, rich in nutrients like omega-3 fatty acids, probiotics, prebiotics, and postbiotics, can help restore the balance of gut bacteria and reduce the risk of mental health problems.
Studies have also highlighted the importance of the gut-brain axis in regulating stress. Maintaining a healthy gut microbiome from an early age can have long-term effects on mental health, potentially reducing the risk of stress-related conditions such as anxiety, irritable bowel syndrome (IBS), and depression.
What causes bad gut health?
Factors like antibiotic use can disrupt this balance, emphasizing the need for maintaining gut health through dietary interventions.
- Antibiotic exposure
- Birth by cesarean section
- Lack of breastfeeding
- Stress exposure
- Infections
The Gut-Immune System Connection
The gut is home to a significant portion of the body’s immune system, playing a vital role in defending against pathogens and maintaining immune homeostasis. A healthy gut microbiota is essential for proper immune function, as imbalances can lead to increased susceptibility to infections, autoimmune disorders, and chronic inflammation, all of which can impact women’s health.
The intricate relationship between your gut microbiome and your immune system operates bidirectionally. Just as the vitality of your immune system can impact the well-being of your gut, the composition of your gut microbiome can directly influence your immune system, particularly with regard to certain forms of inflammation.
How does gut health affect the immune system?
When considering inflammation, it often evokes thoughts of the body’s response to injury such as bruising or cuts. The redness, swelling, and warmth observed during the healing process signify the mobilization of specialized immune cells to combat infection and facilitate tissue repair—a phenomenon known as acute inflammation, an integral aspect of the body’s self-care mechanism.
Contrastingly, chronic inflammation denotes a sustained, prolonged immune response, which can exert detrimental effects on health, predisposing individuals to conditions like obesity, cardiovascular diseases, and type 2 diabetes.
Researchers posit that the gut microbiome serves as a pivotal mediator linking chronic inflammation to these ailments. Over time, consuming inappropriate dietary choices can exacerbate chronic inflammation by precipitating spikes in blood sugar levels and promoting unhealthy lipid profiles.
Scientific investigations have begun unraveling the connection between immune system vitality and specific gut microbes. In a notable study, scientists monitored 2,000 individuals whose gut flora and immune cell counts had been depleted due to chemotherapy and antibiotic treatments. They identified three beneficial microbial strains associated with heightened immune cell levels and two detrimental strains linked to diminished immunity.
Analyzing dietary patterns and immune parameters, scientists observed that consuming ample vegetables correlated with lower levels of pro-inflammatory white blood cells. Additionally, they attributed a portion of this relationship to Collinsella bacteria, which thrive in the presence of processed foods.
Understanding the intricate interplay between gut microbes and immunity underscores the importance of fostering a healthy gut microbiome to bolster immune resilience and mitigate inflammation-related health risks.
Hormonal Balance and Gut Health
Hormonal balance is critical for women’s health, influencing reproductive function, menstrual cycles, mood regulation, and more. Emerging evidence suggests that gut microbiota play a role in hormonal regulation, with certain bacteria involved in metabolizing estrogen and other hormones. Disruptions in gut microbiota can contribute to hormonal imbalances, affecting women’s menstrual health and overall well-being.
Gut health and hormone imbalances are closely connected and can significantly impact overall well-being. Here are some key aspects of their connection:
- Gut microbiome and hormone metabolism: Beneficial bacteria in the gut help break down and eliminate hormones, maintaining a healthy balance. Disruption of the gut microbiome can impair proper hormone metabolism.
- Inflammation and hormonal disruption: Poor gut health can trigger chronic inflammation, disrupting hormone-producing glands and organs, leading to imbalances in estrogen, progesterone, testosterone, and other hormones.
- Nutrient absorption and hormonal balance: A healthy gut lining is essential for optimal nutrient absorption, which affects hormone production.
- Gut-brain axis and hormone regulation: The gut and brain communicate through the gut-brain axis, impacting hormone regulation and mood disorders.
Effect Of Birth Control on Gut Health
Using oral birth control can affect gut health, leading to changes in gut bacteria, leaky gut concerns, nutrient deficiencies, digestive symptoms, mood changes, inflammation, and immune responses. When discontinuing birth control, it can impact gut health by restoring its natural balance.
To restore gut health and promote hormonal balance naturally:
- Identify the root cause of leaky gut.
- Eat a nutrient-rich diet with whole foods and fermented foods while avoiding inflammatory foods.
- Stimulate the vagus nerve through mindful eating and incorporating bitters into your diet.
- Manage stress through meditation, quality sleep, and enjoyable movement.
- Consider targeted supplements like probiotics, immunoglobulins, polyphenols, amino acids, mucosal-support herbs, and zinc carnosine after consulting with a care provider for personalized guidance.
Dietary Impact on Gut Health
Diet plays a significant role in shaping the composition and diversity of gut microbiota. A balanced diet rich in fiber, fruits, vegetables, and fermented foods promotes the growth of beneficial bacteria while reducing the prevalence of harmful microbes. Specific dietary components, such as probiotics and prebiotics, can also directly influence gut health, offering potential therapeutic benefits for women’s wellness.
What is the gut microbiota?
The gut microbiota is a diverse ecosystem of microorganisms in the digestive system. These microorganisms, including bacteria, viruses, fungi, and other microbes, are important for digestion, nutrient metabolism, immune function, and overall health. They interact with the host organism and help maintain a balanced gut environment.
Effect of diet on gut microbiota
The gut microbiota is made up of many different types of microorganisms. They need a variety of nutrients from our diet to stay healthy. When we eat a balanced diet, good bacteria thrive and keep our guts healthy.
- The Role of Dietary Fiber in Gut Health Fiber from fruits, vegetables, whole grains, and legumes is important for the good bacteria in our gut. When these bacteria break down fiber, they make substances that help keep our intestines healthy.
- Polyphenols: Nature’s Gift to Gut Health Polyphenols are found in plant-based foods like berries, green tea, and dark chocolate. They have antioxidants and can help good bacteria grow while stopping bad bacteria from growing.
- Protein and Gut Microbiota Interactions Protein is important for muscles and tissue repair. Eating too much red meat can change the types of bacteria in our gut. Eating more plant-based proteins like legumes, nuts, and tofu can help keep a good mix of bacteria in our gut.
- The Influence of Dietary Fats on Gut Microbiota Diversity Some fats can cause problems in the gut, while others can make it healthier. Omega-3 fatty acids found in fish and seeds are good for the gut.
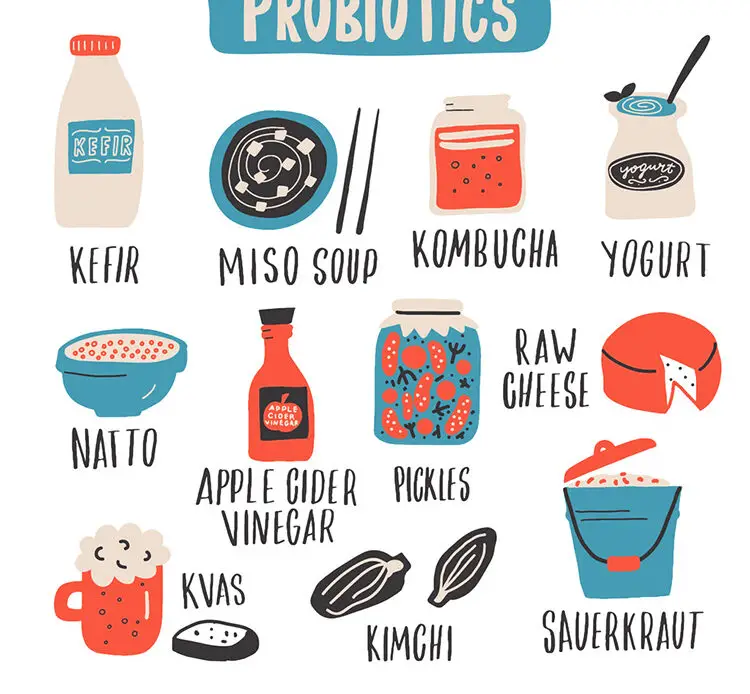
- Fermented Foods: Probiotics for Gut Health Foods like yogurt and sauerkraut have live bacteria that are good for the gut. Eating these foods regularly can help keep a healthy mix of bacteria in the gut.
- Nurturing Gut Health Through Dietary Choices Eating a variety of fiber-rich foods, fruits and vegetables with polyphenols, plant-based proteins, healthy fats, and fermented foods can help keep our gut healthy and improve overall well-being.
Lifestyle Factors and Gut Health
In addition to diet, lifestyle factors such as exercise and stress management play crucial roles in maintaining gut health. Regular physical activity has been shown to promote a diverse gut microbiota and reduce inflammation, while chronic stress can negatively impact gut microbiota composition and function. Adopting stress-reducing techniques such as mindfulness, meditation, and adequate sleep can support a healthy gut and overall well-being for women.
What is causing bad gut microbiota?
Lifestyle factors actively influence gut health. Your diet, exercise routine, stress levels, sleep patterns, and medication use all play pivotal roles in shaping the composition and function of your gut microbiota.
- Diet: Your food choices directly shape the diversity and balance of your gut bacteria. A diet rich in fiber from fruits, vegetables, whole grains, and legumes actively promotes a healthy gut microbiome. Conversely, a diet high in processed foods, sugar, and unhealthy fats actively disrupts gut bacteria, contributing to inflammation and disease.
- Exercise: Regular physical activity actively correlates with a more diverse and beneficial gut microbiota. Exercise actively reduces inflammation, improves digestion, and supports overall gut health. Sedentary behavior, on the other hand, actively decreases gut bacteria diversity.
- Stress: Chronic stress actively alters gut motility, increases intestinal permeability, and disrupts the balance of gut bacteria. Actively engaging in stress management techniques such as meditation, mindfulness, and relaxation exercises can support a healthy gut microbiome.
- Sleep: Poor sleep quality or insufficient sleep actively affects gut health by altering gut microbiota composition and increasing inflammation. Actively prioritizing good sleep hygiene and ensuring adequate sleep duration can support a healthy gut.
- Medication Usage: Certain medications, such as antibiotics, actively disrupt the balance of gut bacteria by actively killing off beneficial microbes along with harmful ones. Other medications, like proton pump inhibitors (PPIs) and nonsteroidal anti-inflammatory drugs (NSAIDs), may also actively impact gut health by affecting digestion and gut lining integrity.
By actively adopting a balanced diet, staying physically active, actively managing stress, prioritizing sleep, and being mindful of medication usage, individuals can actively promote a healthy gut microbiome and actively support overall well-being.
Common Gut Health Issues in Women
Women are more prone to certain gut health issues, including irritable bowel syndrome (IBS), candida overgrowth, and leaky gut syndrome. These conditions can cause digestive discomfort, hormonal imbalances, and immune dysfunction, significantly impacting women’s quality of life. Understanding the underlying causes and implementing targeted interventions is crucial for managing these conditions effectively.
Irritable Bowel Syndrome (IBS)
IBS is a common gastrointestinal disorder characterized by abdominal pain, bloating, diarrhea, and constipation. While the exact cause is unknown, factors such as abnormal gut motility, visceral hypersensitivity, and altered gut microbiota composition are believed to contribute to its development. Women are twice as likely as men to experience IBS, with symptoms often worsening during menstruation.
Candida Overgrowth
Candida is a type of yeast that naturally resides in the gut in small amounts. However, certain factors such as antibiotic use, a high-sugar diet, and weakened immunity can lead to its overgrowth, causing symptoms such as bloating, gas, fatigue, and recurrent yeast infections. Women, especially those taking oral contraceptives or undergoing hormone therapy, are more susceptible to candida overgrowth due to hormonal influences on the vaginal microbiome.
Leaky Gut Syndrome
Leaky gut, also known as increased intestinal permeability, occurs when the lining of the intestinal wall becomes compromised, allowing toxins, bacteria, and undigested food particles to leak into the bloodstream. This can trigger an immune response, leading to inflammation and various symptoms such as food sensitivities, joint pain, skin issues, and autoimmune conditions. Women with conditions like endometriosis and polycystic ovary syndrome (PCOS) may be at a higher risk of developing leaky gut due to chronic inflammation.
Causes of Gut Health Issues in Women
Several factors contribute to the development of gut health issues in women, including hormonal fluctuations, diet and lifestyle factors, and stress.
Hormonal Fluctuations
Estrogen and progesterone, the primary female sex hormones, influence gut motility, secretion of digestive enzymes, and the composition of gut microbiota. Fluctuations in hormone levels throughout the menstrual cycle can exacerbate symptoms of gut disorders like IBS and contribute to bloating, constipation, and diarrhea.
Diet and Lifestyle Factors
The modern diet, high in processed foods, refined sugars, and artificial additives, can disrupt the balance of gut bacteria and contribute to inflammation in the digestive tract. Additionally, factors such as inadequate fiber intake, excessive alcohol consumption, and lack of physical activity can further exacerbate gut health issues in women.
Stress and Mental Health
Women are more likely to experience chronic stress due to various societal pressures, caregiving responsibilities, and work-life balance challenges. Chronic stress can negatively impact gut health by altering gut motility, increasing intestinal permeability, and disrupting the balance of gut microbiota. Furthermore, mental health conditions like anxiety and depression are closely linked to gut health, as the gut-brain axis facilitates bidirectional communication between the gut and the brain.
Symptoms of Gut Health Issues

Bloating and Gas
One of the most common symptoms of gut health issues is bloating and excessive gas. This occurs when there is an imbalance in the gut microbiota, leading to fermentation of undigested food and the production of gases like methane and hydrogen. Bloating can cause discomfort and distension of the abdomen, often accompanied by excessive flatulence.
Abdominal Pain or Discomfort
Persistent abdominal pain or discomfort is another indicator of gut health problems. This may range from mild discomfort to severe cramping, often localized in the lower abdomen. Conditions like irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) can cause chronic abdominal pain and may require medical intervention.
Changes in Bowel Habits
Alterations in bowel habits are often a telltale sign of gut health issues. This includes constipation, characterized by difficulty in passing stools or infrequent bowel movements, and diarrhea, which involves loose or watery stools. Both constipation and diarrhea can disrupt normal bowel function and indicate underlying gastrointestinal problems.
Heartburn and Indigestion
Heartburn and indigestion are symptoms commonly associated with acid reflux, a condition where stomach acid flows back into the esophagus. This can cause a burning sensation in the chest, regurgitation of food, and difficulty swallowing. Persistent heartburn may indicate gastroesophageal reflux disease (GERD), which requires medical evaluation and management.
Maintaining Gut Health for Women
Maintaining gut health requires a multi-faceted approach that encompasses dietary modifications, lifestyle changes, and regular monitoring. Women should prioritize consuming a diverse range of nutrient-rich foods, staying physically active, managing stress effectively, and seeking professional guidance when needed. Regular check-ups and screenings can help identify potential gut health issues early on, allowing for timely intervention and management.
1. Healthy and balanced diet
Maintaining a diverse and balanced gut microbiota is vital. It boosts gut resilience, fights off pathogens, and optimizes nutrient absorption. When this balance is disrupted, known as dysbiosis, it links to obesity, malnutrition, and various diseases.
Diet plays a key role in shaping gut microbiota. Research shows that a diet rich in diverse plant-based foods fosters a healthy microbial balance. Increasing fruit and vegetable intake is a simple way to improve gut health, but adopting a different diet can yield even greater benefits.
Studies highlight the Mediterranean diet’s effectiveness in enhancing the gut microbiome. This plant-based diet includes plenty of vegetables, fruits, whole grains, and olive oil. These foods contain elements that support the growth of beneficial bacteria, promoting reduced inflammation and improved metabolic health.
2. Stress Management
Connection Between Stress and Gut Health
Research has shown that stress can alter the composition and function of the gut microbiota, the community of microorganisms that reside in our intestines. This can weaken the gut’s protective barrier, increase inflammation, and make us more susceptible to digestive disorders. Additionally, stress hormones like cortisol can directly impact gut motility, causing symptoms like diarrhea or constipation.
Effects of Stress on Digestive System
Chronic stress can also impair the production of stomach acid and digestive enzymes, making it harder for the body to break down food and absorb nutrients properly. Over time, this can lead to nutrient deficiencies and other health problems. Therefore, finding effective ways to manage stress is essential for maintaining optimal gut health.
Managing Stress for Better Gut Health
Fortunately, there are many strategies you can use to reduce stress and support your digestive system. Mindfulness practices such as meditation, deep breathing exercises, and yoga have been shown to lower cortisol levels and promote relaxation. Regular physical activity is also beneficial for reducing stress and improving overall well-being.
Stress Reduction Techniques
- Meditation
- Deep Breathing Exercises
- Yoga
- Tai Chi
- Progressive Muscle Relaxation
3. Exercise
Exercise has been shown to enhance the diversity and abundance of beneficial bacteria in the gut, while also reducing the population of harmful microbes. This balance is crucial for optimal gut function and overall health. Moreover, physical activity stimulates the production of short-chain fatty acids (SCFAs), which are vital for gut integrity and immune regulation.
Reduced Risk of Gut Disorders
Engaging in regular exercise has been linked to a lower risk of various gut-related conditions, including inflammatory bowel diseases (IBD), irritable bowel syndrome (IBS), and colorectal cancer. The anti-inflammatory effects of exercise help mitigate chronic inflammation in the gut, thereby reducing the likelihood of developing these disorders.
Improved Digestion Through Physical Activity
Exercise promotes gastrointestinal motility, facilitating the movement of food through the digestive tract. This helps prevent constipation and bloating, leading to improved digestion and nutrient absorption. Additionally, physical activity stimulates the release of digestive enzymes, further optimizing the digestive process.
Enhanced Immune Function
Regular exercise strengthens the immune system, making it more resilient to infections and diseases. A robust immune system is essential for maintaining gut health, as it helps fend off pathogenic invaders and maintains immune homeostasis within the gut mucosa.
Types of Exercises Beneficial for Gut Microbiota
Various forms of exercise can contribute to gut health, including aerobic activities like walking, running, cycling, and swimming, as well as strength training, yoga, and Pilates. It’s essential to incorporate a diverse range of exercises into your routine to reap the full spectrum of benefits for your gut.
Hydration and Gut Health
Proper hydration is essential for maintaining optimal gut function during exercise. Water helps transport nutrients, regulate body temperature, and lubricate the digestive system. Drink plenty of fluids before, during, and after exercise to stay hydrated and support healthy digestion.
Gut Health and Women’s Longevity
Maintaining optimal gut health is not only essential for addressing immediate health concerns but also for promoting longevity and healthy aging. By supporting immune function, hormonal balance, and mental well-being, a healthy gut can contribute to a higher quality of life and increased longevity for women as they age.
In women, gut health plays a crucial role in hormonal balance, immune function, digestive health, and mental well-being. Hormonal fluctuations throughout a woman’s life, such as those experienced during menstruation and menopause, can affect gut health and vice versa.
Strategies for Improving Gut Health
Adopting lifestyle habits that promote a healthy gut is essential for women’s longevity. This includes consuming a balanced diet rich in fiber and probiotics, practicing stress management techniques, engaging in regular physical activity, and prioritizing quality sleep.
Specific Foods for maintaining good gut microbiota
Certain foods are particularly beneficial for gut health, including fiber-rich foods like fruits, vegetables, and whole grains, as well as fermented foods like yogurt, kefir, and sauerkraut. Prebiotic foods, which contain fiber that nourishes beneficial gut bacteria, and foods rich in omega-3 fatty acids, such as fatty fish and flaxseeds, also support gut health.
Digestive Health During Pregnancy and Postpartum
Pregnancy and postpartum are critical periods during which gut health can significantly impact both maternal and fetal health. A healthy gut microbiota is essential for nutrient absorption, immune function, and metabolic regulation during pregnancy.
Recommended Supplements For Gut Health
Supplementation can play a significant role in sealing up leaky gut and restoring the integrity of the gut lining. Here are some key supplements and nutrients that can support this process:
- Probiotics: I recommend spore-based probiotics and specific strains such as Lactobacillus rhamnosus, L. reuterii, and Bifidobacterium longum to re-seed the gut and support hormonal balance.
- Immunoglobulins: Consider immunoglobulins to help with dysbiosis and regulate the immune response.
- Polyphenols: Incorporate polyphenol-rich foods and supplements to strengthen the gut barrier. Amino acids and mucosal-support herbs: Support the gut lining by consuming amino acids like L-proline, L-serine, L-cysteine, and L-threonine, along with herbs such as marshmallow, slippery elm, aloe vera, okra, and licorice.
- Zinc Carnosine: Take zinc carnosine to enhance gut integrity and healing.
Frequently Asked Questions
- What are the main causes of gut health issues?
- Gut health issues can arise due to various factors, including poor diet, stress, medications, and underlying medical conditions.
- Can gut health problems affect mental well-being?
- Yes, there is growing evidence of the gut-brain connection, indicating that gut health can influence mood, cognition, and mental health.
- When should I see a doctor for gut health issues?
- If you experience persistent or severe symptoms such as abdominal pain, changes in bowel habits, or unexplained weight loss, it’s essential to consult a healthcare professional for evaluation and management.
- Are there any natural remedies for improving gut health?
- Yes, incorporating probiotic-rich foods, fiber-rich fruits and vegetables, and fermented foods like yogurt and kefir into your diet can promote gut health naturally.
- Can stress affect gut health?
- Yes, stress can disrupt the balance of gut microbiota and increase the risk of gastrointestinal problems. Practicing stress management techniques such as meditation, yoga, and deep breathing exercises can help support gut health.
- Can any type of exercise benefit gut health?
- While all forms of exercise offer some degree of benefit, activities that combine cardiovascular exercise with strength training tend to be most effective for promoting gut health.
- How soon can I expect to notice improvements in my gut health through exercise?
- The timeline for experiencing improvements in gut health varies from person to person and depends on factors such as the individual’s current gut microbiome composition, exercise intensity, and dietary habits. Consistent exercise coupled with a balanced diet can lead to noticeable improvements within a few weeks to a few
References
- Sekirov, I., Russell, S. L., Antunes, L. C., & Finlay, B. B. (2010). Gut microbiota in health and disease. Physiological reviews, 90(3), 859-904.
- Mayer, E. A., Knight, R., Mazmanian, S. K., Cryan, J. F., & Tillisch, K. (2014). Gut microbes and the brain: paradigm shift in neuroscience. Journal of Neuroscience, 34(46), 15490-15496.
- Round, J. L., & Mazmanian, S. K. (2009). The gut microbiota shapes intestinal immune responses during health and disease. Nature Reviews Immunology, 9(5), 313-323.
- Parodi, A., Paolino, S., Greco, A., Drago, F., & Mansi, C. (2015). Small intestinal bacterial overgrowth in rosacea: clinical effectiveness of its eradication. Clinical Gastroenterology and Hepatology, 13(4), 875-876.
- Hill, C., Guarner, F., Reid, G., Gibson, G. R., Merenstein, D. J., Pot, B., … & Sanders, M. E. (2014). Expert consensus document: The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nature Reviews Gastroenterology & Hepatology, 11(8), 506-514.
- Kuo, S. M. (2013). The interplay between fiber and the intestinal microbiome in the inflammatory response. Advances in Nutrition, 4(1), 16-28.
- Yang, Y., Zheng, W., Cai, Q., Shrubsole, M. J., Pei, Z., Brucker, R., … & Shu, X. O. (2020). Dietary fiber intake and risk of breast cancer by menopausal and estrogen receptor status. European journal of nutrition, 59(7), 3069-3080.
- Magrone, T., Jirillo, E., & Spagnoletta, A. (2019). Emerging role of gut microbiota in the control of inflammation and tolerance in allergy. Current medicinal chemistry, 26(25), 4854-4869.
- Molina-Torres, G., Rodríguez-Arrastia, M., Roman, P., Sánchez-Labraca, N., & Cardona, D. (2017). Stress and the gut microbiota-brain axis. Behavioural pharmacology, 28(2 and 3-Spec Issue), 140-151.